Key takeaways:
- Drug giant Eli Lilly and OpenAI are partnering to leverage AI to find new antibiotics that can kill superbugs.
- Overuse of antibiotics to treat people, animals and plants has led to a rise in drug-resistant antibiotics.
- MIT has taken on this initiative since 2020, discovering antibiotics that can kill the dreaded MRSA and other deadly bacteria.
Pharma giant Eli Lilly is partnering with OpenAI to use its generative AI technology to invent new antibiotic drugs that can fight drug-resistant bacteria.
Lilly is stepping up its efforts through its social impact AMR Action Fund, which is investing $100 million to develop two to four new antibiotics by 2030 and contribute to related causes.
With the frequent use of antibiotics to treat people, animals and plants, some deadly bacteria strains have become immune. Such antimicrobial resistance has long been a critical threat to public health, but the pipeline for new antibiotics is thin because it doesn’t make as much money as other drugs, according to a paper in Nature.
Diogo Rau, the drugmaker’s chief information and digital officer, said in a statement that “generative AI opens a new opportunity to accelerate the discovery of novel antimicrobials and the development of custom, purpose-built technologies” to fight drug-resistant pathogens.
The collaboration between Lilly and OpenAI potentially opens new avenues for pharmaceutical innovation and patient care to reshape the landscape of antimicrobial research and development.
MIT’s discoveries
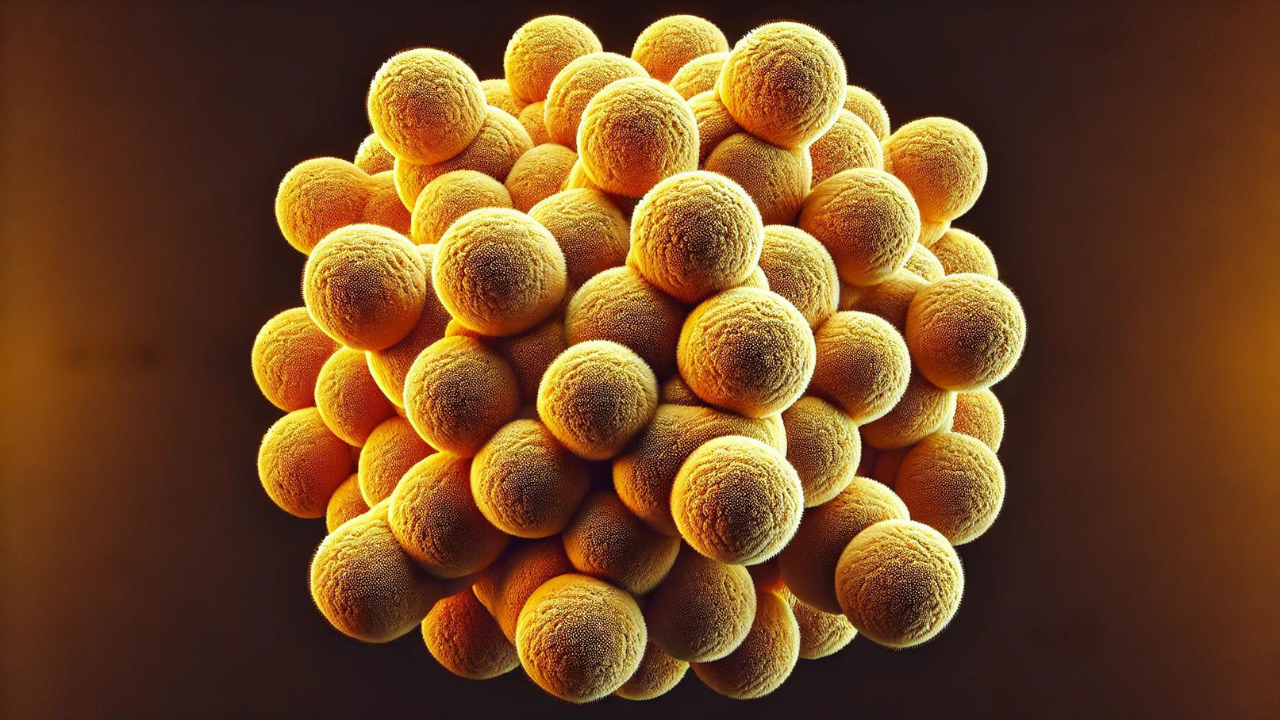
Last December, MIT researchers used deep learning to discover a class of compounds that can kill the dreaded MRSA (methicillin-resistant Staphylococcus aureus) while posing low toxicity to human cells, according to a paper published in Nature.
The researchers’ trained a deep learning model on data they generated by testing 39,000 compounds for its antibiotic strength against MRSA. A new molecule was then given to the model, which offered a probability that the compound is antibacterial. To further narrow down the drug candidates, the team trained three other deep learning models to predict whether the compound is toxic to humans.
“The insight here was that we could see what was being learned by the models to make their predictions that certain molecules would make for good antibiotics,” said James Collins, an MIT professor of medical engineering and science, in MIT News. “Our work provides a framework that is time-efficient, resource-efficient, and mechanistically insightful, from a chemical-structure standpoint, in ways that we haven’t had to date.”
The endeavor is part of MIT’s Antibiotics-AI Project, whose mission is to discover new classes of antibiotics to fight seven of the world’s deadliest bacteria over seven years. They are the Escherichia coli, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, Neisseria gonorrhoeae, Staphylococcus aureus, and Mycobacterium tuberculosis.